It is estimated that there are over 300 million cases of hip and knee OA worldwide with prevalence of the disease increasing with age. The main risk factors of developing OA include being overweight, having diabetes, lack of physical activity, occupation and physical load, hip shape, prior traumatic injury and more.
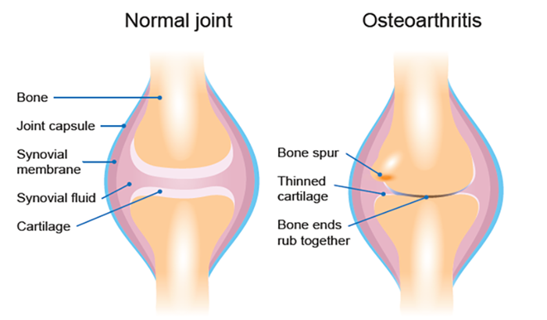
Simply put, OA is a change in the bone structure overtime which causes damage to the soft cartilage that helps disperse weight through the joint and cushion bone contact when weight-bearing. Damage to the cartilage can lead to other issues in the joint, and changes in bone structure can result in reduced range of movement, pain with daily activities, involving the lower limb, and general soreness in the area especially first thing in the morning.
The symptoms of advanced OA are commonly addressed with joint replacement which involves major surgery to increase compatibility of the two bony surfaces that make up the joint. This can be costly and lead to long periods of recovery and requires rehabilitation to get you back to your pre-operative level of function.
A less invasive way to prevent the development of symptoms and help manage them is through physiotherapy. There is a lot of evidence which states that regular activity and strengthening of the surrounding muscles will lead to a decrease in pain and increased function. The highest level evidence recommends a combination of cardiorespiratory exercise, strengthening exercise and balance training regularly. There is also high level evidence for the use of Topical non-steroidal anti-inflammatory drugs (NSAIDs) but it is best to see your doctor or pharmacists before use to see if this is suitable for you.
As physiotherapists we can educate you about the disease and its progression as well as recommend specific exercises that will suit your situation, taking into factor other health issues you may be dealing with. We also recommend giving exercise a go before jumping into surgery as it can only provide a positive result. Going into surgery stronger, will result in better conditions post surgery, you could progress in such a way that you no longer need surgery or could delay it for a long period. The more you delay surgery, the less chance of you needing to go in for another replacement or review in the future. It is also noted that 1 in 5 report an unfavourable pain outcome after surgery meaning that surgery may not relieve your symptoms as you would expect, and that 25% of total knee replacements won’t last 25 years.
Moral of the story; give physiotherapy a try! It can only be beneficial whether you choose to have surgery or not and it could save you time, pain and money.
Peat, G., & Thomas, M. J. (2021). Osteoarthritis year in review 2020: epidemiology & therapy. Osteoarthritis and Cartilage, 29(2), 180-189.
Bannuru, R. R., Osani, M. C., Vaysbrot, E. E., Arden, N. K., Bennell, K., Bierma-Zeinstra, S. M. A., … & McAlindon, T. E. (2019). OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis and cartilage, 27(11), 1578-1589.
Berenbaum, F. (2013). Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!). Osteoarthritis and cartilage, 21(1), 16-21.
What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients BMJ Open, 2 (2012), p. e000435
Evans, J. T., Walker, R. W., Evans, J. P., Blom, A. W., Sayers, A., & Whitehouse, M. R. (2019). How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. The Lancet, 393(10172), 655-663.